A Revolutionary Idea Whose Time Has Come…
If we can create Opioid Replacement Therapy to save lives from heroin…
If we can make Nicotine Replacement Therapy to help smokers quit…
Then why — in a society where alcohol kills over 3 million people per year — do we still have nothing that safely replaces alcohol’s effects?
Where is the Alcohol Replacement Therapy (ART)?
This isn’t a crazy idea. It’s common sense. It’s neuroscience. It’s harm reduction.
And honestly, it’s long overdue.
🧠 What I Mean by “Alcohol Replacement Therapy”
⚗️ When I say “Alcohol Replacement Therapy,” I’m talking about a medically guided, harm-reduction-based system that gives people access to non-toxic, receptor-targeted alternatives to alcohol.
⚡ In other words, it’s a harm-reduction approach that targets the same neural pathways alcohol hijacks—but with safer, smarter chemistry 🔬.
Think of how Opioid Replacement Therapy (ORT) works:
Buprenorphine or methadone replaces heroin or fentanyl — engaging the same opioid receptors,
reducing cravings and withdrawal, without the chaos or lethality.
Or how Nicotine Replacement Therapy (NRT) works:
Patches, gum, and pouches provide controlled nicotine doses without tar and carbon monoxide.
🌍 Both of these save millions of lives.
🧠 Both normalize the nervous system instead of punishing the person.
🤔 So why not alcohol?
🚫 The Gaping Hole in Modern Addiction Medicine
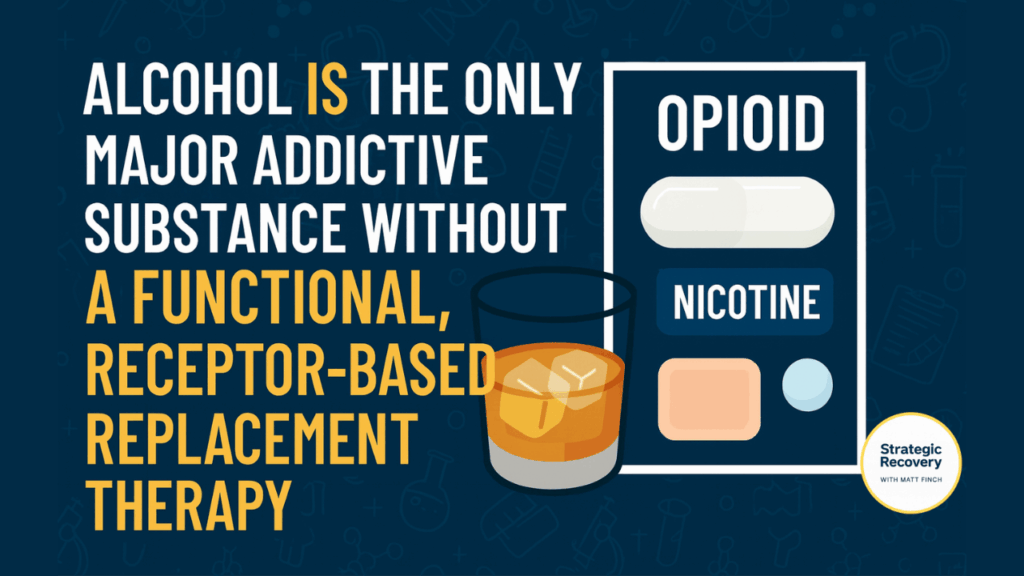
Here’s the brutal truth: Alcohol is the only major addictive substance without a functional, receptor-based replacement therapy.
Not for lack of science — we know exactly what alcohol does.
It primarily activates GABA-A receptors (relaxation, sedation) and dopamine pathways (reward and motivation).
We also know dozens of compounds that interact with these systems. So where’s the medication? Where’s the innovation?
Instead, the system still clings to outdated ideas:
“Just say no.” “Go to meetings.” “Use willpower.”
And if you can’t? You’re labeled as “noncompliant.”
Medical Reality Check 🩺
Stigma vs. Science💉 Imagine if we told diabetics to stop insulin “cold turkey.”
🫁 Or if we told someone with asthma to “just breathe better.”
🍺➡️🧠 That’s what we’re doing to millions suffering from Alcohol Use Disorder (AUD).
💊 The Science of Substance Replacement Therapy
Replacement therapy is not about getting high.
It’s about stabilizing neurochemistry so that people can heal.
- Opioid Replacement Therapy (ORT): Buprenorphine and methadone bind to opioid receptors, preventing withdrawal and reducing cravings. Buprenorphine’s ceiling effect makes overdose almost impossible (SAMHSA).
- Nicotine Replacement Therapy (NRT): Patches, gum, or vapes replace the delivery system without the combustion damage (American Cancer Society).
- Alcohol Replacement Therapy (ART): …Does not exist. Yet.
And yet, research shows that when receptors are balanced, the nervous system can rewire. The brain can finally relax. The person can think clearly, sleep deeply, and begin true recovery.
This is harm reduction. This is compassion. This is science.
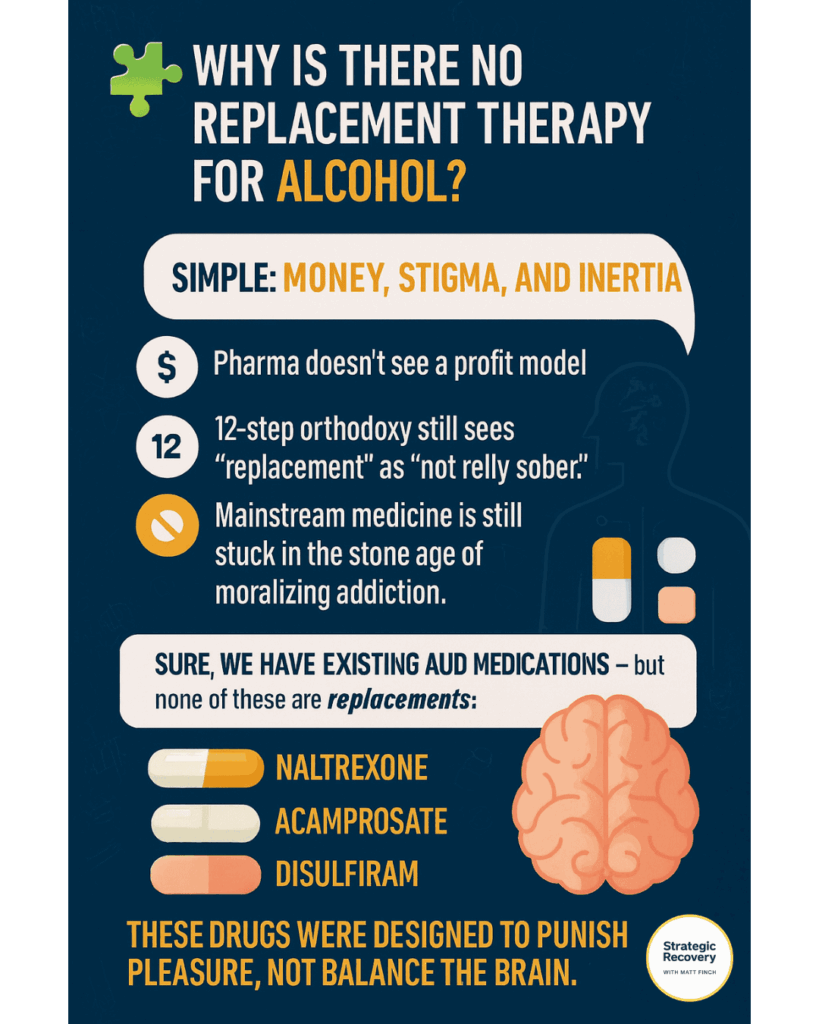
🧩 Why Is There No Replacement Therapy for Alcohol?
Simple: money, stigma, and inertia.
Pharma doesn’t see a profit model.
12-step orthodoxy still sees “replacement” as “not really sober.”
And mainstream medicine is stuck in the stone age of moralizing addiction.
Sure, we have Naltrexone, Acamprosate, and Disulfiram — but none of these are replacements.
Why the Old Approach Punishes Pleasure — and the New One Heals It
❌ Punish Pleasure
These legacy drugs suppress or shame the brain’s reward system instead of restoring it:
- Naltrexone blocks pleasure — it doesn’t replace it.
- Acamprosate is too weak to rebuild reward pathways.
- Disulfiram punishes drinking through sickness — aversion therapy from the 1950s.
✅ Balance the Brain
The next generation of care focuses on restoring balance, not suppressing reward:
- Baclofen — supports calm and confidence through GABA-B activation.
- Gabapentin / Pregabalin — eases anxiety and restores sleep quality.
- Low-Dose Naltrexone (LDN) — rebalances reward pathways for true neuroplastic healing.
We don’t need to punish the brain for wanting joy.
We just need to teach it how to find it again. 💛
Educational only, not medical advice.
⚗️ What Could Alcohol Replacement Therapy Look Like?
Imagine a medicine that:
- Binds gently to GABA-A or GABA-B receptors
- Reduces anxiety and withdrawal
- Restores normal dopamine and serotonin function
- Has a built-in ceiling effect to prevent abuse
- Supports neuroplasticity and emotional healing
We already have hints in nature and science:
- Baclofen – A GABA-B agonist that reduces cravings for some (NIH).
- Phenibut HCL – A GABA analog developed by Soviet scientists (effective but banned by FDA).
- Clonazepam (and other benzos) – Works, but risky for dependency.
- Kava – Natural GABAergic herb with promising anti-anxiety effects (Science Direct).
- L-Theanine + Lemon Balm + GABA + Magnesium – Gentle synergistic combo that mimics mild alcohol relaxation.
✨ We’re not far off.
💡 We just need innovation without stigma — science guided by compassion, courage, and common sense.
🕊️ True healing begins when wisdom replaces fear… and love leads the way.
⚡ The DIY Era: Harm Reduction in Action
I’ve experimented with this concept myself — both in the past and through my recovery coaching practice.
My own early version of “Alcohol Replacement Therapy” looked like:
🧊⚡💊 Red Bull on the Rocks + 5 mg Diazepam
This mix hit the GABA-A receptors (for calm) and dopamine (for focus). 🧭 It gave me balance, not intoxication.
Later, I found Phenibut even more effective — until the FDA banned it. It was, hands down, one of the most powerful tools I’d ever seen for reducing alcohol cravings, social anxiety, and insomnia. But like anything powerful, it carried risk if abused.
And that’s the point: The potential is there. The need is there. The science is there. What’s missing is courage and compassion. ✊💛
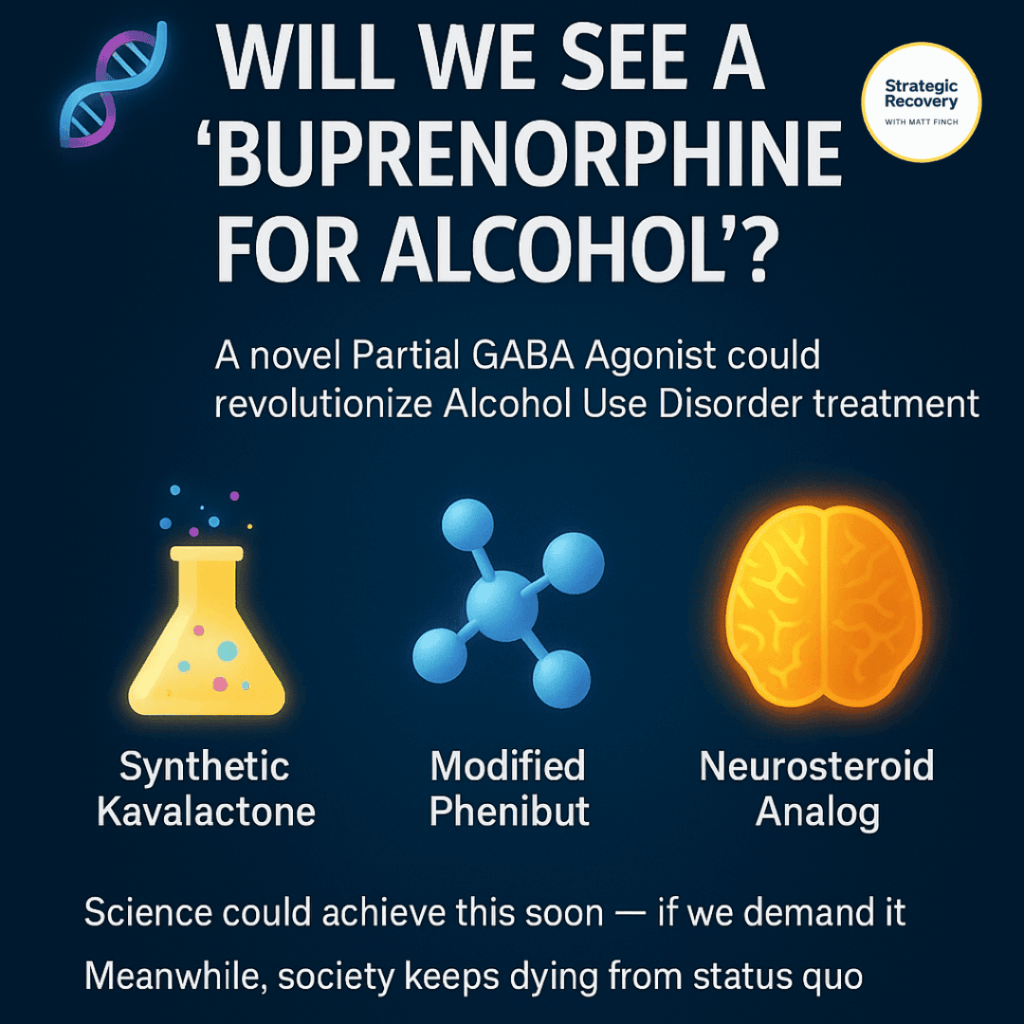
🧬 The Future: Will We See a “Buprenorphine for Alcohol”?
We could — and we should.
A long-acting, partial GABA agonist with a ceiling effect, mild dopamine modulation, and low toxicity could revolutionize Alcohol Use Disorder treatment.
Maybe it comes from synthetic kavalactones.
Maybe from a modified Phenibut molecule.
Maybe from a novel neurosteroid analog.
Science can do this tomorrow — if the system demands it.
But until then, people will keep dying needlessly from the world’s most socially acceptable poison.
🧬 The Buprenorphine Question: Could It Work for Alcohol Too?
On a biochemical level, buprenorphine already checks many of the boxes that an “Alcohol Replacement Therapy” drug would need.
It’s a partial opioid agonist — meaning it stimulates endorphin and dopamine release just enough to stabilize the system, but not enough to cause euphoria or intoxication (by using a “therapeutic dose”).
And here’s the wild part: nearly everyone I’ve met or coached who’s on buprenorphine for opioid use disorder tells me their desire for alcohol vanishes completely.
No cravings. No social drinking impulse. No reward-seeking itch. Just peace.
So… what gives?
Why hasn’t the FDA explored this connection?
Why is no one running large-scale studies on buprenorphine for Alcohol Use Disorder (AUD) — even though we have millions of real-world “case studies” showing its effect?
Off-Label Reality Check Buprenorphine & AUD
Doctors can prescribe buprenorphine off-label for pain, depression, or even treatment-resistant fatigue.
So technically, yes — they could prescribe it off-label for alcohol dependence.
But in reality? Most physicians won’t risk it. The system makes it legally possible but professionally radioactive.
Insurance barriers. DEA scrutiny. Outdated moral frameworks. We have a medication sitting in plain sight that could save lives — but bureaucracy and stigma block the door.
Maybe what we really need isn’t more molecules… It’s more courage inside the system to try what already works.
🌿 Kratom: The Underground Alcohol Replacement
Now, step outside the medical model for a moment.
Enter the underground lab of the human spirit: self-treatment.
Every week, I hear from people who’ve traded nightly drinking for a few grams of kratom — and haven’t looked back.
They tell me:
“I don’t even want alcohol anymore. It feels pointless.”
🧬 Kratom’s alkaloids (mitragynine, 7-hydroxymitragynine) target endorphin and dopamine pathways — similar to opioids, but with gentler, more modulated effects.
🧠 From a logical standpoint, this makes perfect sense.
Humans self-medicate to balance their neurochemistry — and for many, kratom offers a softer, natural bridge to fill the gap that alcohol leaves behind.
⚖️ Kratom: The Double-Edged Remedy
But of course, there are caveats.
🪜 For some, kratom becomes the ladder out of a pit — for others, another hole to climb out of.
Like any powerful tool, it’s about strategy, self-awareness, and biochemical individuality.

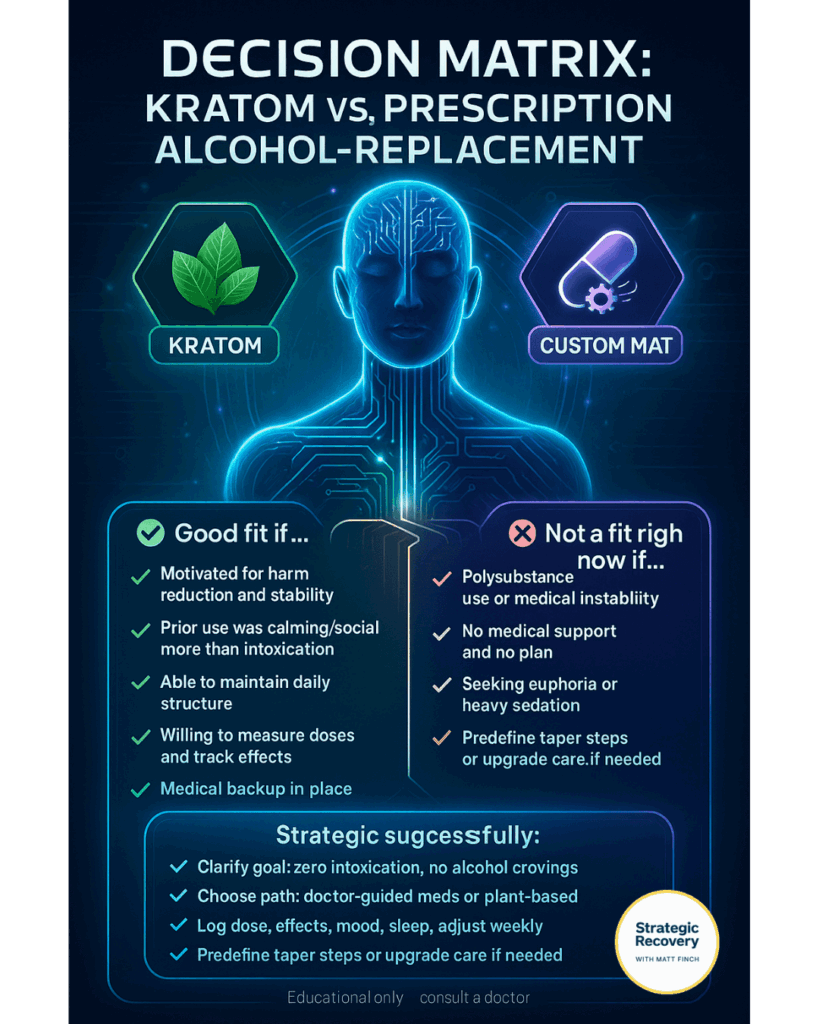
🧭 Decision Matrix: Kratom vs. Prescription Alcohol-Replacement
Use this quick matrix to sense-check your fit. Everyone’s biochemistry, history, and risk profile are different — choose the path that maximizes safety and stability.
- You’re highly motivated for harm reduction and stability (not a “buzz”).
- Past alcohol use was about calming/social ease more than heavy intoxication.
- You can keep simple daily structure (sleep, meals, hydration, supplements).
- You’re willing to use measured doses, track effects, and adjust strategically.
- You have medical backup (PCP or addiction MD) for questions and monitoring.
- History of opioid/benzo dependence or compulsive use patterns.
- Multiple unresolved mental-health stressors (panic, trauma, insomnia) without support.
- Uncertain product quality or legal status in your area.
- You struggle to keep doses consistent or skip days to “feel it.”
- Active polysubstance use with recent overdoses or severe medical instability.
- No access to trusted medical care, no plan, and high-risk environment.
- You’re seeking euphoria or heavy sedation rather than receptor balance.
🧠 If “Yes,” here’s a Strategic Plan
- Clarify the goal: zero intoxication, steady mood, sleep repair, no alcohol cravings.
- Pick a lane: Doctor-guided (eg, baclofen, gabapentin, carefully managed clonazepam) or self-directed plant path (eg, standardized kratom; start low, go slow).
- Stack supports: electrolytes, magnesium glycinate, omega-3s, protein breakfast, sunlight + walks.
- Dosage & diary: log time, amount, effects, sleep, cravings, mood (1–10 scale). Adjust weekly.
- Safety rails: no mixing with alcohol, benzos, or opioids; lock in weekly check-ins with a trusted person.
- Exit plan: pre-define taper steps if tolerance creeps up or goals are met (eg, 10–20% reduction weekly).
- Upgrade care: if cravings persist or anxiety spikes, consult an addiction MD for off-label options (baclofen, gabapentin/pregabalin, cautious short-term clonazepam, or evaluation for other MAT).
Educational only — not medical advice. Work with a clinician when possible, especially if you have other conditions or take prescriptions.
🩺 Can My Doctor Help Me Off-Label?
Here’s where the rubber meets the road.
If you’re seeking Alcohol Replacement Therapy, the most strategic first step isn’t necessarily kratom or black-market self-experimentation — it’s finding a doctor who actually listens.
Off-Label Toolkit
Doctor-Guided OptionsMany people don’t realize this: physicians can legally prescribe certain medications off-label — when there’s a reasonable scientific basis and a clear therapeutic goal. 💡
Clonazepam (Klonopin) — GABA-A receptor modulation for calm without intoxication (only if tightly managed).
Baclofen — GABA-B activation; may reduce cravings & social anxiety.
Gabapentin / Pregabalin — balances glutamate–GABA; supports sleep & eases withdrawal stress.
Low-dose Naltrexone (LDN) — may help reset reward pathways and support neuroplastic recovery.
Catch: most mainstream doctors haven’t heard the phrase “Alcohol Replacement Therapy.” Many are trained in abstinence-only frameworks — not receptor restoration.
⚠️ Educational only, not medical advice. If this resonates, bring notes to your clinician and discuss risks, benefits, and monitoring.
🧭 How to Talk to Your Doctor
Use this roadmap to collaborate with your provider for personalized recovery solutions.
-
1️⃣Prepare. Bring data, studies, and this article. Print it out.
-
2️⃣Advocate. Tell your story clearly — what you’ve tried, what worked, what didn’t.
-
3️⃣Collaborate. If your doctor’s unsure, suggest a referral to an addiction-medicine specialist.
-
4️⃣Persist. Sometimes it takes three or four “no’s” to find one “yes.”
🤝 If that doesn’t work…
There’s a growing network of progressive telehealth providers — a new generation of doctors who understand harm reduction, neurochemistry, and personalized recovery.
They’re not just treating addiction.
They’re treating the human behind it. 💛
⚖️ Risk, Reward, and the Art of Strategic Recovery
So — buprenorphine, baclofen, clonazepam, kratom… which is “best”?
There’s no universal answer. Only a strategic one.
Every human brain is a different ecosystem — shaped by trauma, genetics, neurochemistry, and environment.
The right tool for one person could be the wrong one for another.
That’s why the decision isn’t moral.
It’s mathematical.
If the risk of drinking outweighs the risk of a replacement, that’s not addiction — that’s harm reduction wisdom.
If a safe medication or plant can normalize your neurotransmitters, prevent relapse, and give your brain a chance to heal — why would we withhold it?
The truth is, recovery doesn’t have to mean deprivation.
It can mean balance, peace, and stability — through science, self-knowledge, and compassion-driven strategy.
That’s what Strategic Recovery is all about:
- 🧠 Smart. Evidence-guided and mechanism-aware.
- 💛 Loving. Dignity-first, shame-free, human-centered.
- 🌍 Revolutionary. Systems-level change that restores reward, not punishes it.
🕯️ Final Thoughts: Science + Spirit + Sanity
Let’s call it what it is:
The recovery industry has failed to innovate.
Millions of lives have been lost because of dogma and disinterest.
Meanwhile, brilliant harm-reduction researchers, underground biohackers, and recovery mavericks are already experimenting with solutions that work.
It’s time to elevate this conversation.
Alcohol Replacement Therapy should exist.
It should be studied, funded, tested, and refined.
Because no one deserves to die from a treatable imbalance in brain chemistry.
The future of recovery isn’t about abstinence alone.
It’s about alignment, innovation, and compassion.
Let’s build it — together.
Key Takeaways
- ✅ Replacement therapy works — proven with opioids and nicotine.
- 🚫🍺 Alcohol is the outlier — the only major drug without a receptor-based replacement.
- 🧪 We already have promising templates (Baclofen, Phenibut, Kava, etc.).
- 🛟 Harm reduction saves lives. Dogma costs them.
- 🤝 True recovery meets people where they are — biochemically, emotionally, spiritually.
Call To Action
If this vision resonates with you, share this article.
Let’s start the global conversation about Alcohol Replacement Therapy — because the future of recovery depends on it.
- 🔗 Copy the link and send it to someone who’d understand.
- ✉️ Email it to a clinician, policymaker, or journalist.
- 💬 Quote a line on social and tag a few allies.
Alcohol Replacement Therapy (ART): The Science, Vision & Compassion Behind the Movement
A deep dive into why ART should exist, what it could look like, and how harm reduction can reshape recovery forever.
What is Alcohol Replacement Therapy (ART)?
Why does alcohol need a replacement therapy?
How would ART actually work in the brain?
What could a future ART medicine look like?
What compounds or plants point the way to ART?
Why hasn’t the system developed this yet?
What can people do now while waiting for ART?
🌌 Join the Recovery Renaissance
Be part of the movement redefining recovery through
wisdom, science, and compassion.
Every step you take toward balance helps light the way for others. 🌠




Leave a Reply